Introduction
According to the Baylor College of Medicine, about 40 infectious diseases have been discovered since the 1970’s. These include SARs, MERS, Ebola, swine flu, Zika and COVID-19. This suggests that as we continue moving past the major disruptions to our daily lives caused by the pandemic, there may be future infectious diseases requiring attention to increase transmission prevention. Resultant of the massive public health education initiatives during the pandemic, we are intimately familiar with the importance of various transmission prevention techniques including handwashing, social distancing, and wearing masks. Also, we are aware of the necessity of avoiding contact with those having symptoms of infectious illnesses. Although symptoms vary dependent upon the infectious disease, common ones are fever, diarrhea, fatigue, muscle aches and coughing.
The need to avoid contact can be challenged if you are called upon to offer transportation to a medical clinic or even the local emergency department for a feverish friend or family member who doesn’t reside in your household. Have you thought about how you’ll handle a request for nonemergency transport? What measures will you take to keep you and your sick passenger safe? Do you know what items they will need upon arrival to the medical facility? What’s the best way to minimize time spent with them to decrease your exposure time as well as get them to a place of effective treatment? Should you even accept responsibility for this transport, or would the person be better served by calling 911? Here are some thoughts to consider before possibly placing yourself as an unintentional vector by transporting an ill individual or even going into their home. It is human nature to want to help, but it’s wise to consider the potential health risks to yourself as well as to those in your household.
Compelling Reasons for Wanting to Help
Living through this pandemic has left many concerned that direct contact with individuals with communicable diseases threatens not only those having the actual encounter but potentially creates vulnerability within their community. Despite risks, there are many compelling reasons to provide transportation to someone with an actual or possible infectious disease.
One is the innate desire to help others, which transcends across most cultures and religions. This is evident globally by the outpouring of support and assistance from multiple groups anytime there is a disaster resulting in human suffering. That same desire emerges when someone we love and care about has a need. Providing transportation to a person with a possible infectious disease might help in eliminating suffering and feelings of isolation and fear.
Another reason is many of us operate on some level of Quid Pro Quo, the giving of goods or services because of the expectation of getting something back in return. We may not expect or desire reciprocation from the one assisted. However, there can be a nagging concern if we do not help; we could later find no one is willing to give us needed assistance. Whether labeled karma, kismet, or reaping what you sow, it can be an influencing factor in making the decision to help someone.
Cost and availability of transportation services are also reasons for considering assisting. This varies greatly depending upon what types of ride shares, taxis or non-emergency medical transportation companies are available within the community. Some provide exactly what is needed. Others have limited hours of daily operation and/or policies prohibiting the transport of someone with a suspected or actual infectious disease. While most places across the nation do offer ambulance services, this can be very pricey. While the cost to the transported individual depends on where they live and if they have insurance, the price tag of an ambulance ride ranges from a few hundred dollars to $1,277 or more.
Finally, we may feel compelled to assist because we fear there is no one else available. This concern may not be unfounded as a 2021 report released by the United States Census Bureau identifies there are over 37 million or 15% of all US adults age 18 and over living alone. Also, even those living with others might reside with household occupants unable to assist because they are dependent children, disabled, or are ill themselves.
Transportation and Contact Considerations
In critical situations such as chest pain or other sudden onset of new pain, shortness of breath or uncontrolled bleeding, the transportation method is calling 911 Emergency Services. Otherwise, if you decide to transport the individual, you’ll need to contemplate if you or someone else in your household is in a high risk category should disease transmission occur.
The term, high risk individuals, is something the public has heard much about since the advent of COVID-19. How do you know if you or someone in your household is at high risk of becoming infected from whatever illness has befallen your passenger?
According to Centers for Disease Control and Prevention (CDC), certain medical conditions, and medicines used for treatment, may make someone more susceptible to severe illness and possibly death. Cancer, diabetes, chronic lung conditions, and high blood pressure are a few examples of underlying health conditions that could worsen should you or a household member become infected.
Even if an underlying disease is not a concern, there are possible disruptions and inconveniences resulting from a minor change in plans to a more significant work-around situation. For instance, if you become sick, how long can you afford to be off from your job? What about changing an approaching medical or dental procedure should you fall ill? Do you have upcoming travel plans? Immediate travel plans even without infectious disease exposure restrictions can be complicated if illness strikes during your trip. These challenges can include not knowing where to access care at your destination site or having to pay higher costs because of receiving care outside of your insurer’s approved network of providers. Make a quick mental note of your own unique situation and how your choice whether to help transport is worth the risk for yourself and those closest to you.
Prior to agreeing to transport someone, consider how much time you are able to reasonably devote to this endeavor. Whether the destination is a healthcare provider’s office, urgent care or hospital emergency department, it can be challenging calculating the amount of time needed. Even in settings where given an appointment and/or approximate wait time, delays arise quickly due to such events as a sudden influx of patients or a patient’s emergent need requiring multiple staff members’ full attention. Therefore, you and your potential passenger need to explore alternative transport modes in the event that restrictions arise. These potential restrictions might include work obligations or the need to pick up children within a short period of time.
Before and After Transport
After making the decision to transport the person, determine if you have access to necessary items such as facial coverings including masks or respirators or face shields. Also needed in your vehicle are gloves, tissues, and a trash receptacle. A plastic bag next to the ill passenger is a must in case of vomiting. Have hand sanitizer containing at least 60% alcohol in the car. Paper towels and disinfecting wipes are necessary supplies for transport.

Upon arrival for pickup, if they have symptoms suggestive of a respiratory infection such as coughing, wheezing or sneezing both you and your transport need to be wearing masks or respirator prior to face to face contact. Maintaining a calm demeanor and speaking in an unhurried and reassuring manner helps set the tone for a much more relaxed transport.
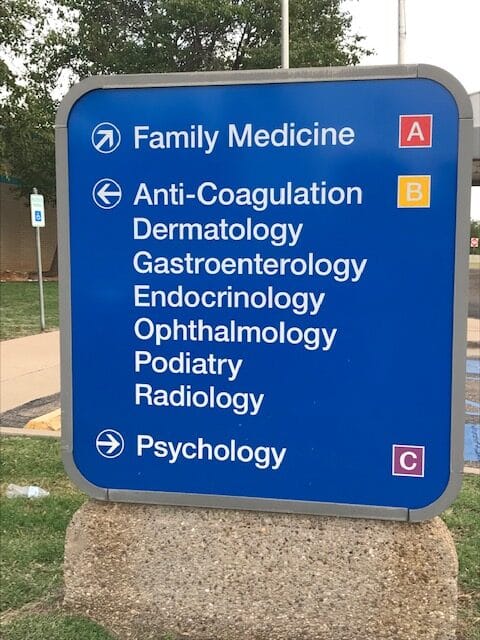
Before departing for the facility to which the person has requested transport, there are several considerations. Obtaining answers may require visiting the facility’s website or calling the specific department to which your passenger is directed. Questions include: Does the facility accept someone with active signs of infection, such as coughing, fever, or diarrhea? If so, are there specific instructions concerning entering the facility such as where to check in? Does the facility accept their insurance? What are the payment requirements at the time the services are rendered? Can a same day appointment be made? Obtaining answers may save wait time and exposure length to someone with a possible infectious disease. Also, it may prevent delays in being seen, which can be a more comfortable and kinder alternative than waiting in either a vehicle or facility’s holding area.

Before leaving their home, offer to make phone calls to relatives or neighbors if they have young children, elderly, or pets needing care while away. Also, confirm the person has a current and complete list of all medications, including over-the-counter, herbal supplements and prescriptions. They need their government-issued identification card, insurance, and/or Medicaid and Medicare cards with them. Assist with packing an overnight bag of such essentials as toothbrush, toothpaste, house slippers, phone charger and reading material. Of course, check with the facility before bringing in personal care items, as the person might be placed in isolation. Make sure they have their eyeglasses, hearing aids, dentures, and other assistive devices needed to function safely. Bring a copy of their Living Will and Power of Attorney if available. Ask them if they want you to call anyone such as a family member or work manager to apprise them of the situation. With their permission, store their significant other’s contact information in your phone in the event you have questions or concerns.
Upon entering your vehicle it is prudent for both your passenger and yourself to wear masks or respirators. During transport, to minimize exposure to a possible infection, a study published in a January 2021 Issue of Science Advances suggests an ill passenger ride in the backseat, diagonal the driver, with windows rolled down, weather permitting.

After transport, clean and disinfect surface areas within your vehicle. Before using any type of cleaning or disinfecting products, check your vehicle manufacturer guidelines concerning the care of the interior. Dispose of tissues and anything else the person used in the car. While cleaning and disinfecting the interior surfaces within in your vehicle, wear gloves and mask or respirator and wash your hands upon completing the task.
Although in many situations transmission risk of infectious agents from skin, hair, and clothing is minimal, there are several personal hygiene considerations following the transport. While appropriate for anyone wanting to minimalize the risk of transmission, they are especially important if contact with someone from a high risk group occurs shortly after the transport. Safest measures includes upon returning home immediately changing and laundering clothes, plus showering and shampooing hair.
Final Thoughts
Preventing disease transmission has always been and remains a challenge with the potential of yet unknown germs attempting the establishing a stronghold by infecting unsuspecting people. One of the pandemic’s lessons many have learned is social distancing from those displaying signs of infectious diseases. Deciding whether or not to transport someone who is ill and resides outside your household requires considering the risks associated with not being able to maintain social distancing between yourself and those within your inner circle.
Remember, it’s ok to say no. If unable to be the one providing transport, you can still render assistance by calling 911 Emergency Services or perhaps enlisting the assistance of a less vulnerable friend or family member. At times though, someone’s need is so compelling concerns about transporting become secondary to getting a person to the place where they can receive help. If faced with that situation, having a plan for transport using information discussed in the previous paragraphs can prove very beneficial and help to not become an unintentional vector.
When determining what to do, it is helpful to remember that the safest transport is the one where the infectious disease risk is minimized and the ill person receives the needed level of care. Such actions ensure a positive outcome for all involved.
By Phyllis Hooten and Tonya Warren

Phyllis Hooten,
Phyllis, a PhD prepared nurse, has experience as a nurse scientist and nursing instructor at both the graduate and undergraduate levels. She currently is a grant writer at Anchor Advising, LLC and a freelance writer. She has been lead or co-author of over 20 articles, mostly in peer reviewed professional healthcare journals. Most recently she has been published in Nursing 2022, Mysterious Ways, Texas Public Health Journal, American Nurse, and Archives of Psychiatric Nursing.

Tonya Warren
A nurse of 34 years, Tonya has a vast knowledge of medical-surgical patient care and is currently enjoying her Preadmission Testing department where she prepares patients and families for an upcoming procedure or surgery to achieve the best possible outcomes. Tonya is also a freelance writer utilizing her people skills to tell the story of her subjects and the difference they make in our world.

